The immune system’s response to reactivated human cytomegalovirus (hCMV) infection, a form of herpes virus, has been linked to the onset of graft-versus-host disease (GVHD).
The discovery, made by a research team at the VCU Massey Cancer Center in Virgina, suggests that these genetic markers may help identify patients at risk of developing GVHD, a life-threatening complication of bone marrow or stem cell transplants.
The study, “Sequence homology between HLA-bound cytomegalovirus and human peptides: A potential trigger for alloreactivity,” appeared in the journal PlosOne.
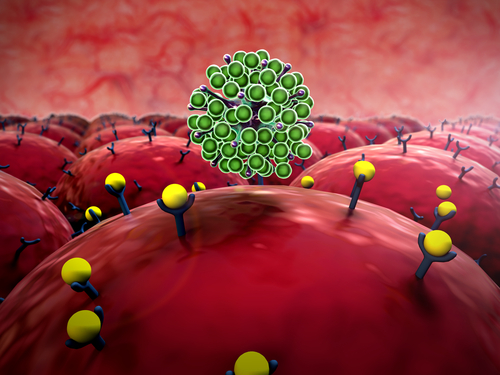
hCMV is a virus that has evolved with humans for over thousands of years. The virus remains dormant in the body after the initial infection, without major impact on a person’s life.
It is estimated that 50 to 80 percent of the U.S. population has been infected with hCMV by the age of 40, and the majority are hardly bothered by it. But for people with a weakened immune system, including those who undergo transplants, the virus can pose a serious risk.
In a stem cell transplant, a patient’s immune system is replaced by cells of a matched donor. During this process, 30 to 65 percent of patients experience a reactivation of hCMV, which has been linked to GVHD. The connection between hCMV reactivation GVHD onset, however, is poorly understood.
Led by Amir Toor, an hematologist-oncologist in the Bone Marrow Transplant Program at the Massey center, researchers examined hCMV markers in the DNA of 77 matched stem cell donors and transplant recipients. Eighteen patients, post-transplant, had hCMV reactivation and GVHD development, including 13 who showed newly active hCMV prior to GVHD.
The researchers found a pattern of genetic hCMV markers that were present in tissues affected by GVHD. Specifically, they found similarities between human peptides — short amino acid chains that act as regulators of the immune response — seen in GVHD-affected tissues and those related with hCMV. Using computer-based modeling, they showed that the immune system of transplant patients could promote GVHD in response to the virus-similar peptides.
“We developed a computer model that shows how the immune system can react to hCMV peptides to trigger a graft-versus-host response,” Toor said in a news release, and a way to “further identify patients at risk and better personalize post-transplant care to decrease the potential for graft-versus-host disease.
“Until now, physicians have taken a ‘wait and see’ approach to antiviral therapies following transplantation,” he added. “But, based on our data, we believe there is a case for early intervention with personalized antiviral treatments following stem cell transplantation in order to suppress hCMV reactivation.”
Researchers plan to further explore their findings and predictive hCMV-GVHD computer modeling analysis in a larger group of stem cell donor and recipient pairs.
This study was partially supported by funding from a NIH-NCI Cancer Center Support Grant awarded the Massey Cancer Center.