Adding vorinostat to the standard treatment used during high-risk stem cell transplants might reduce rates of acute transplant rejection, according to a small Phase 2 trial.
Since the study also indicated the approach as safe, the results, published in the journal Blood, support testing the treatment in a large Phase 3 trial.
The study, “Vorinostat plus Tacrolimus/Methotrexate to Prevent GVHD 1 Following Myeloablative Conditioning Unrelated Donor HCT,” used the combination of vorinostat (sold as Zolinza for cutaneous T-cell lymphoma) to tacrolimus and methotrexate. All three are FDA-approved therapies.
The approach had been tested with promising results in patients who received a milder preparative treatment — called a conditioning regimen by doctors — before the transplant, which was donated by a relative.
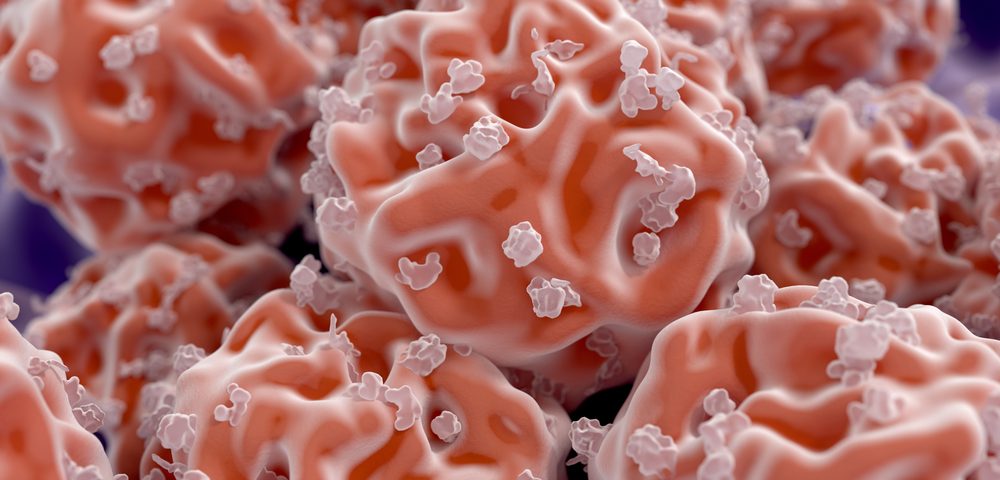
But researchers from Michigan Medicine at the University of Michigan noted that most patients do not have a suitable relative to donate bone marrow. And when a transplant is received from an unrelated person, the procedure is much more risky, with graft versus host disease (GVHD) developing in 50 percent to 70 percent of patients who are treated with standard immunosuppressive drugs.
Graft versus host disease is the scientific name used when the donor’s immune system attacks the recipient’s healthy tissues.
Using unrelated donors also usually requires a harsher pretreatment, and the Phase 2 clinical trial (NCT01790568) included 37 patients who would receive a bone marrow transplant after so-called myeloablative conditioning — meaning the bone marrow was completely wiped out before the transplant.
They all received bone marrow from an unrelated donor as part of their blood cancer treatment. Among them, 73 percent had acute myeloid leukemia, and researchers judged that nearly 20 percent had high-risk disease.
The treatment with 100 mg vorinostat, twice daily, was started 10 days before the transplant. At 100 days after the transplant, 22 percent had developed moderate or severe acute GVHD, of which 8 percent had more severe disease. Twenty-nine percent also developed chronic GVHD.
The findings compare favorably with other studies reporting an incidence of 50 to 60 percent of acute graft versus host disease in AML patients 100 days after transplant, and a 25 percent incidence of severe disease.
One year after the transplant, 47 percent had survived without developing transplant rejection or cancer relapse, and 76 percent were alive. No patient experienced a transplant failure.
The treatment was well tolerated, with side effects similar to those reported in earlier studies of the drug.
The findings support advancing the treatment approach to larger, Phase 3 clinical trials.