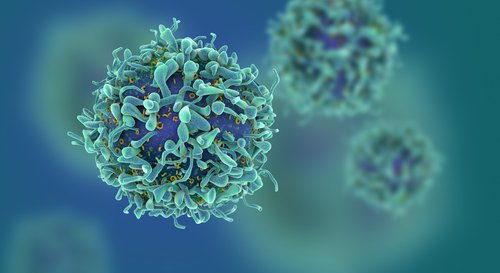
Controlling the balance of two subsets of immune T-cells, known as CD4+ and CD8+, after stem cell transplants makes it possible to prevent graft-versus-host disease (GVHD) while keeping the anti-cancer activity of the healthy transplanted cells, results from a preclinical study show.
The study, titled “PD-L1 interacts with CD80 to regulate graft-versus-leukemia activity of donor CD8+ T cells,” was published in the Journal of Clinical Investigation.
In many cases of leukemia and lymphoma, patients require what is called as allogeneic hematopoietic cell transplantation (HCT) to fight the cancer. By removing the tumor cells from the body and replacing them with healthy cells from a donor, HCT can prevent the cancer from relapsing. But this therapeutic strategy can lead to GVHD, a life-threatening side effect where the donor cells attack the patient’s healthy tissues.
“Currently, immunosuppressive drugs have been used to prevent GVHD, but immune-suppressants also subdue the anti-cancer effects of the donor T-cells, potentially resulting in cancer relapse, in addition to other side effects such as an increased risk of infection,” Defu Zeng, senior author of the study, said in a press release. “Therefore, prevention of GVHD while preserving anti-cancer effects remains the ‘holy grail’ of allogenic HCT.”
According to a research team led by City of Hope investigators, a temporary depletion of CD4+ T-cells from the donor after HCT procedure will exhaust the donor’s CD8+ T-cells, inhibiting them from attacking the recipient’s body. At the same time, the process enhances the anti-cancer activity of the donor CD8+ T-cells.
Tightly controlling these T-cell subsets may therefore induce strong graft-versus-leukemia/lymphoma (GVL) effects without the negative effects of GVHD.
“If successfully translated into clinical application, this regimen may represent one of the novel approaches that allow strong GVL effects without causing GVHD,” Zeng said. “This kind of regimen has the potential to promote wide-spread application of allogenic HCT as a curative therapy for hematological malignancies.”
Following these results, Zeng and his collaborators are working on a new therapy that could efficiently delete CD4+ cells. He hopes to take this new therapeutic regimen into clinical trials.