Targeting B-cell lymphoma using genetically modified natural killer T-cells — rather than general T-cells — may be a more effective, cheaper, “off-the-shelf” immunotherapy, a preclinical study suggests.
The study, “Enhanced Anti-lymphoma Activity of CAR19-iNKT Cells Underpinned by Dual CD19 and CD1d Targeting,” was published in the journal Cancer Cell.
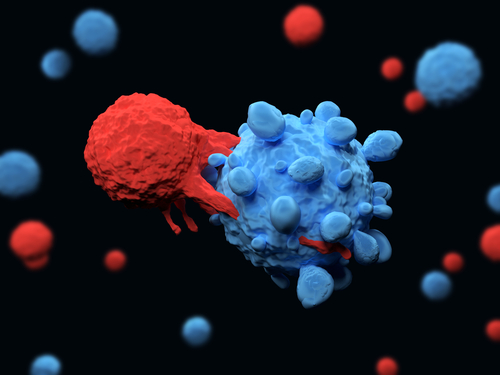
Chimeric antigen receptor (CAR) T-cell therapy is currently one of the most promising strategies to fight cancer. It consists of genetically altering T-cells — a type of white blood cell that recognizes foreign molecules through specific membrane receptors — so their receptors specifically recognize and kill tumor cells.
CAR T-cell therapy requires taking blood from the patient, isolating T-cells, changing the cells genetically to attack proteins associated with cancer, and then infusing them back into the patient.
While this approach has shown very positive results in patients with blood cancers who have no other chance of cure, a significant proportion of patients still relapse, highlighting the need to improve the effectiveness of CAR-based immunotherapy.
In addition, current CAR T-cell therapies are very expensive — about $400,000 per patient — and time-consuming, since they are mainly developed from the patient’s own cells to prevent immune reactions against the cell therapy.
Using the same approach but with natural killer T-cells (NKT) may solve these issues. This subpopulation of T-cells have an intrinsic anti-tumor activity and have been shown to suppress immune reactions against stem cell transplants from donors other than the patients themselves.
CAR T-cell therapy against B-cell cancers has mainly been based on the addition of a receptor against CD19, a protein highly present in the cell surface of malignant and healthy B-cells.
NKT cells already have a receptor that recognizes a protein present in many subtypes of malignant B-cells — called CD1d — and the addition of a modified receptor that recognizes CD19 could potentially enhance an immune response against malignant B-cells.
Researchers at Imperial College London and King’s College London evaluated whether this approach, called CAR19-iNKT therapy, led to better results in fighting B-cell lymphoma than similar CAR-T therapy (CAR19-T-cell therapy). Their work was funded by the U.K. blood cancer charity Bloodwise.
First, they developed an optimized protocol to produce CAR19-iNKT cells, which required fewer cells to be modified before being expanded, and less reagents during the process of genetic modification, which is expected to significantly reduce the overall cost of their production.
Also, the ability to generate these cells from healthy donors would enable one batch of cells to be used on several patients, and in a shorter period of time.
The team then compared the anti-tumor effects of CAR19-iNKT and CAR19-T-cell therapies in cells grown in the lab and in mice with B-cell lymphoma.
The results showed that CAR19-iNKT cells were more effective than CAR19-T-cells at eliminating cancer cells, both in cells grown in the lab and in mice. A significantly greater proportion of mice treated with CAR19-iNKT cells were cancer-free and survived for a longer period of time than those treated with CAR19-T-cells.
“This effect is associated with a significantly more robust anti-tumor effect in the first few days post immunotherapy, perhaps a reflection of the physiological role of iNKT cells as the immune cells that modulate an emerging immune response well before conventional T-cells,” the researchers wrote.
To the researchers’ surprise, CAR19-iNKT cells were also able to reach the brain and eradicate brain lymphoma, which CAR19-T-cells could not do.
These findings suggest that CAR19-iNKT cells are an effective therapy for B-cell lymphomas, and that iNKT cell-based immunotherapy could be an effective therapeutic approach for other types of blood cancers and brain cancers.
“The possibility of cheaply mass-producing highly effective anti-cancer immune cells is in many ways the holy grail of CAR therapy,” Alasdair Rankin, Bloodwise’s director of research, said in a press release. “If successful, it would open up these life-saving treatments to many more patients.”
According to Antonia Rotolo, the study’s first author, the next step is to test this approach in clinical trials, where they can assess the therapy’s potential side effects.