European patients with non-Hodgkin’s lymphoma (NHL) are more likely to receive rituximab biosimilars if they are fitter, have indolent disease, or follicular lymphoma, according to a new study.
The study, “Treatment approach for non-Hodgkin lymphoma patients since first biosimilars of rituximab approved in EU5,” was presented at the 2018 American Society of Clinical Oncology (ASCO) Annual Meeting, held June 1-5 in Chicago, Illinois.
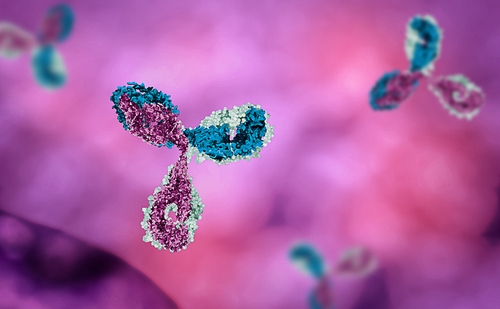
Since its debut in the U.S. in 1997, Rituxan (rituximab) has been used to treat many forms of B-cell lymphomas. Patients may receive the antibody either to eliminate the cancer — usually in combination with chemotherapy — or to extend the time until it comes back.
More recently, in 2017, the first rituximab biosimilars were approved by the European Medicines Agency (EMA) to treat NHL: Truxima in February, followed by Rixathon and Riximyo in June, and Blitzima, Ritemvia, and Rituzena in July.
Biosimilars are biological medical products that are nearly identical to the original product, but manufactured by a different company once the original patent expires. They usually are sold at significantly lower prices, but the patterns of biosimilar prescriptions in NHL patients is not known.
This online, multi-country, multi-centre medical review study analyzed how rituximab biosimilars are being prescribed in five European countries to determine if they are preferred over branded medications for treating specific types of patients.
The study analyzed prescription data from 97 physicians who treated a total of 640 patients with NHL in France (117), Germany (73), Italy (117), Spain (136), and United Kingdom (197) between July and September 2017. Prescription data included date of diagnosis, current and historic patient treatment, and reasons for prescribing or discontinuing anti-cancer drug treatment.
From the 640 patients analyzed, 77% were treated with a therapeutic regimen that included branded rituximab. The prescription rates of rituximab biosimilars were highest in Germany and the United Kingdom, where 14% and 13% of patients, respectively, were treated with a rituximab biosimilar.
The use of biosimilars in these countries increased toward later lines of treatment, with only 11% of patients receiving rituximab biosimilars as a frontline treatment ,compared with 18% and 30% who received it as a second- and third-line of treatment, respectively.
Comparing German and U.K. patients who took standard rituximab and rituximab biosimilars, investigators found that those receiving biosimilars were more likely to be fitter (able to perform at least light daily activities), have slow-growing disease, and have no comorbidities affecting cancer treatment.
These patients also more were likely to have follicular lymphoma.
Altogether, the data suggest that in Europe physicians are more likely to prescribe rituximab biosimilars to healthier NHL patients who have the indolent form of the disease or follicular lymphoma.