A gene therapy-based cancer treatment completely eliminated traces of tumor cells in 40 percent of patients with certain B-cell malignancies, according to data from a Phase 1/2a clinical trial.
The study also showed that increased levels of immunosuppressive cells were predictive of treatment failure and decreased survival.
The data, presented at the recent CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference: Translating Science into Survival, in Frankfurt, Germany, was from a Swedish study that used third-generation CAR T-cell therapy to target CD19-positive cells.
The U.S. Food and Drug Administration has already approved Novartis’ CAR T-cell therapy as the first gene therapy-based cancer treatment for children and young adults with B-cell acute lymphoblastic leukemia.
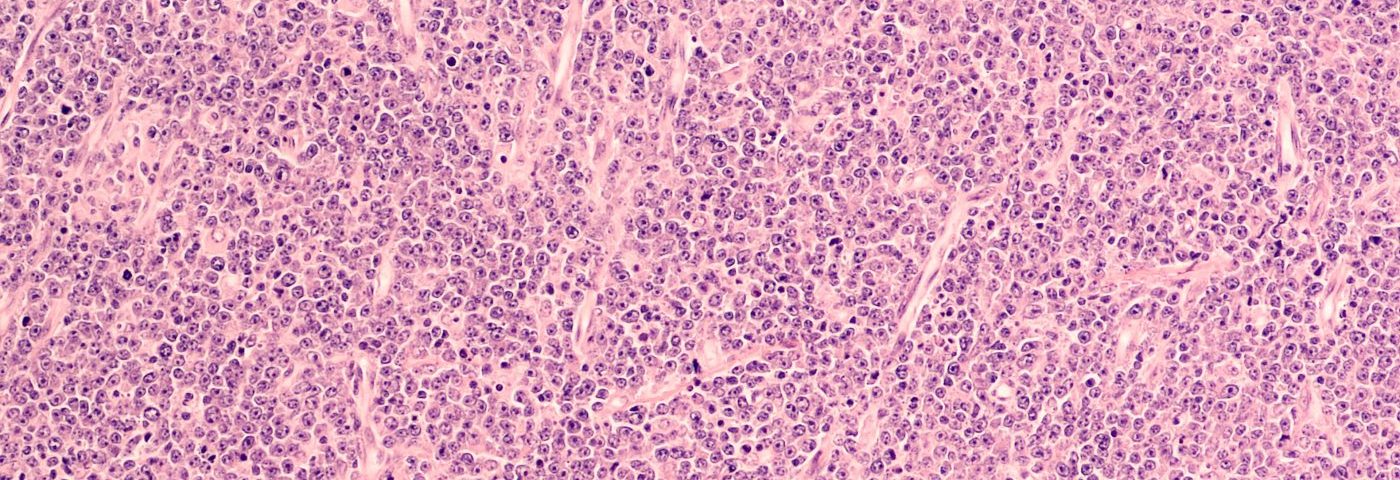
The therapy turns the patient’s own immune cells into aggressive fighters of malignant cells that have a surface receptor called CD19.
The third-generation CD19-specific CAR T-cell therapy was tested in 15 patients with CD19-positive, B-cell malignancies who had relapsed on or after prior treatment. Eleven patients had lymphoma and four had leukemia.
Results showed that six patients, or 40 percent, had a complete response to treatment, meaning all tumors were gone. These responses lasted for a median of five months, but even the four patients who relapsed responded well to subsequent therapy.
Serious adverse events were observed in four patients, three of whom had cytokine-release syndrome, a life-threatening condition characterized by an overactivation of the immune system.
Toxicity related to the central nervous system (the brain and spinal cord) occurred in two patients. All serious adverse events either resolved on their own or with treatment.
There is an ongoing search for biomarkers that are associated with disease evolution to track patient responses to CAR T-cell therapy. This study identified a series of factors that correlated either with better or worse overall survival.
“We set out to investigate the safety and effectiveness of a third-generation CD19-specific CAR T–cell therapy and to identify potential biomarkers of treatment outcome,” Tanja Lövgren, PhD, a researcher in the Department of Immunology, Genetics and Pathology at Uppsala University in Sweden, said in a press release. “We found that the treatment was generally safe and effective, and that an immunostimulatory environment was associated with improved overall survival while immunosuppressive cells and factors were associated with treatment failure and decreased overall survival.”
Lövgren pointed out that further studies are needed to confirm the results. They indicate that a combination of CAR T-cell therapy with immune checkpoint inhibitors or other drugs that mitigate the immunosuppressive environment within tumors might be a good approach for such patients.
Lövgren noted that the study had limitations. These included the small scale of the study, the fact that several different types of B-cell malignancy were involved, and that some patients may have been too ill to respond to any treatment.
“We are hoping to follow up this study with another clinical trial that will combine CAR T-cell therapy with chemotherapy known to decrease the number of monocytic myeloid-derived suppressive cells,” Lövgren said . “We are also looking to further optimize the CAR T-cell therapy.”