University of Illinois researchers have learned how cells that surround bone marrow help a certain type of stem cell produce all of the body’s blood cell types.
Mimicking the three-dimensional bone marrow tissue environment in the lab may help researchers grow large numbers of the hematopoietic stem cells. That could lead to a higher rate of transplant success in patients with blood diseases.
A key finding of the research is that a factor in the cells surrounding blood marrow, or the extracellular matrix, controls whether the stem cells proliferate. Another revelation was that a different factor controls whether stem cells evolve into other types of cells — a change that means they are unable to produce blood cells.
The study, “Marrow-inspired matrix cues rapidly affect early fate decisions of hematopoietic stem and progenitor cells,” was published in Science Advances.
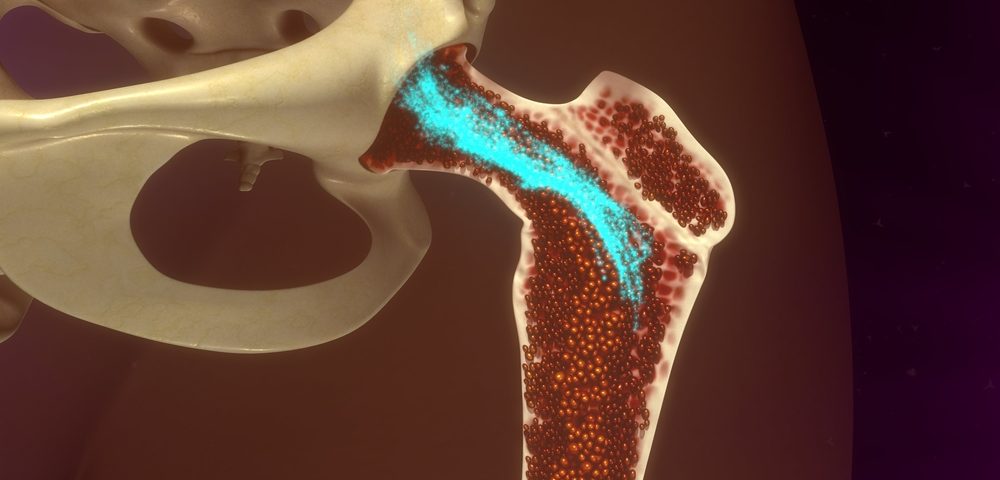
Hematopoietic stem cells, which are the precursors of all blood and immune cells, are found in bone marrow regions called niches. There they receive a variety of signals that determine their fate — whether they will proliferate or evolve into other cells, for example.
“The tissue environment that surrounds these cells in the bone marrow provides a wealth of signals that can alter how these precursor cells behave. This paper looked at the signals provided by the tissue matrix itself,” Brendan Harley, a biomolecular engineering professor at the University of Illinois’ Carl R. Woese Institute for Genomic Biology, said in a press release.
Transplanting hematopoietic stem cells remains one of the major treatments for patients with blood diseases, like leukemia and lymphoma. The transplanted cells must travel to the bone marrow to produce blood and immune cells. The current state of medicine means that the number of stem cells obtained from a donor is limited, and the transplant success rate low.
“We’re interested in this problem from an engineering standpoint,” Harley said. “The goal is to create better tools to both expand the number of donor HSCs [hematopoietic stem cells] and improve their capacity to repopulate the bone marrow after transplantation.”
Harley and postdoctoral researcher Ji Sun Choi wanted to know how the extracellular matrix influences the stem cells’ ability to proliferate and evolve into other cells. Stem cells that evolve lose their ability to produce both blood and immune cells.
The researchers used engineered biomaterials with different compositions of extracellular matrix to grow stem cells from mice in a laboratory. They paid particular attention to two main elements of the bone marrow extracellular matrix, collagen and fibronectin.
When the stem cells were cultured in collagen-based three-dimensional structures, they proliferated rapidly, but they also differentiated, or evolved into other cells — meaning they lost their ability to generate blood and immune cells. When they were cultured in fibronectin, they proliferated slower, but maintained their stem cell properties.
“With the collagen substrates, we got more cells but not useful cells,” Harley said. “With the right combination of stiffness in the matrix and the presence of fibronectin, we identified a class of biomaterials that show promise for being able to maintain and eventually expand these stem cells outside of the body. An engineered bone marrow will be of enormous value for treating hematopoietic cancers such as leukemia, but also for understanding the process of bone marrow failure and other hematopoietic diseases.”
The researchers’ work was a first step toward understanding how the extracellular matrix controls the fate of hematopoietic stem cells. Harley is now studying other characteristics of this complex environment that could be used to increase bone marrow transplant success rates.