A new study has identified the transcription factor FOXP1 as the main regulator in cancer cells’ ability to evade immune responses in patients with diffuse large B-cell lymphomas (DLBCL). The study, which identified the novel molecular relationship between FOXP1 and genes essential to immune response, is titled “FOXP1 suppresses immune response signatures and MHC class II expression in activated B-cell-like diffuse large B-cell lymphomas” and published in Leukemia.
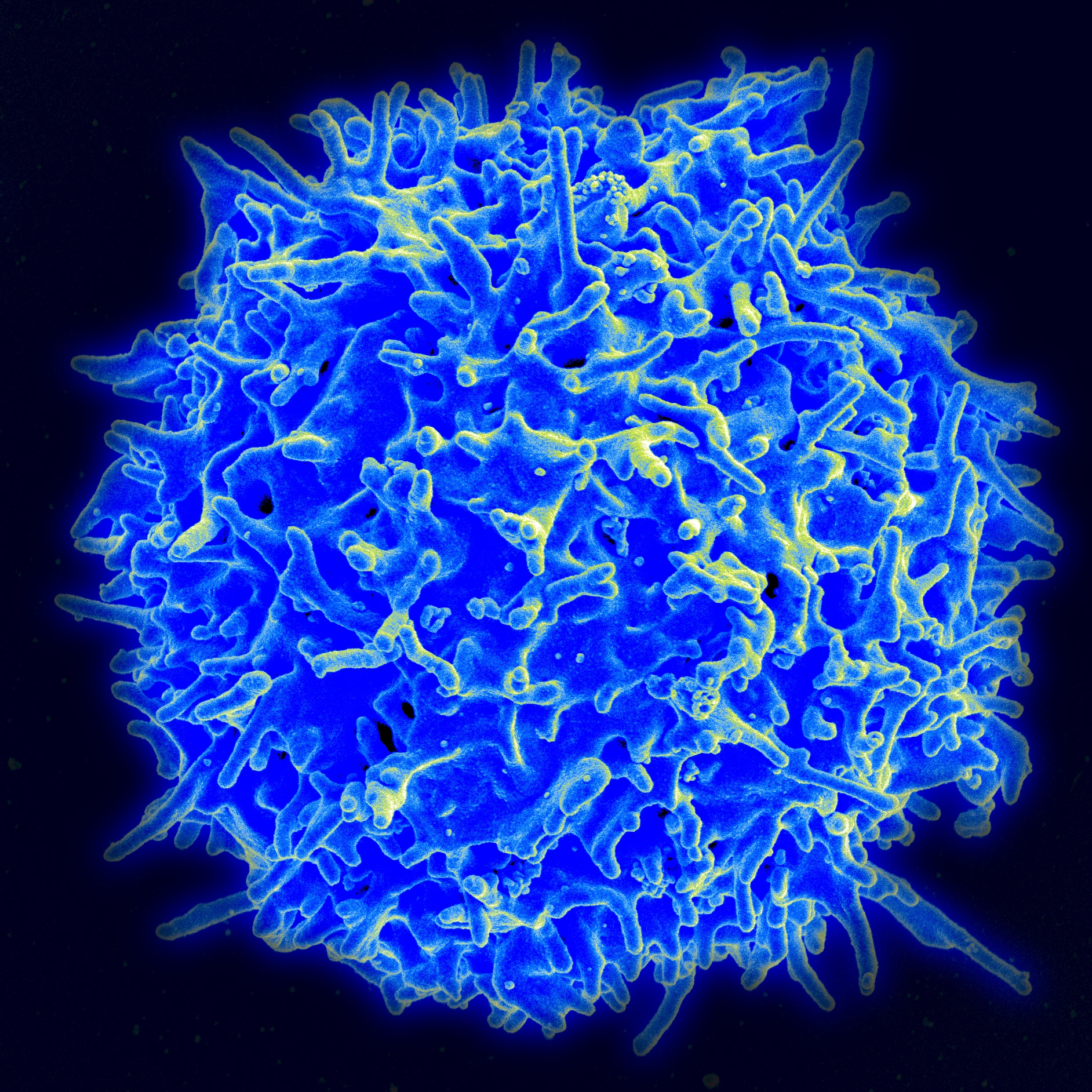
DLBCL are malignancies characterized in the clinic through their genetic and molecular profiles. The use of biomarkers allows clinicians to attribute personalized treatments and predict a patient’s response to molecular-targeted therapies. One of these markers is FOXP1, a transcription factor (switches genes on and off) involved in the development of B cells, a type of white blood cell extremely important for the correct functioning of the adaptive immune system response.
FOXP1 has been shown to promote tumor cell suppression in breast cancer and other malignancies, while an oncogenic role has been proposed in the context of lymphoma. Several relevant molecular pathways have been established for FOXP1, including one that relates FOXP1 expression to overall levels of major histocompatibility complex (MHC) II: low tumor MHC II levels are associated with shorter survival rates in lymphoma patients, probably as a consequence of low levels of antigen-presenting cells allowing tumor cells to go undetected by the immune system.
In this study, Oxford University researchers silenced the FOXP1 gene in a particular subset of DLBCL cells, where short forms of FOXP1 are abundant, observing that MHC II proteins’ surface expression, namely HLA-DRA, was higher. Moreover, researchers compared tumor molecular profiles of 150 DLBCL patients and found that in those with high HLA-DRA expression, 72% survived longer than five years, while in patients with low expression of HLA-DRA only 38% achieved this survival rate.
RELATED: Why We Need Clinical Trials For Lymphoma
This research highlights the importance of FOXP1 in tumor cell evasion of the immune system, which could be used to explore new gene therapy approaches where, for example, the FOXP1 gene can be silenced in lymphoma cells to allow an efficient immune response by the patient’s own immune cells.
Said Dr. Matt Kaiser, head of Research at Bloodwise, the researchers’ funding institution, of these promising results in a press release: “Understanding how the FOXP1 protein enables tumor cells to hide from the immune system could be a significant step in improving outcomes for hard-to-treat cases. Diffuse large B-cell lymphoma is the most common type of blood cancer and is responsible for a considerable loss of life each year in the UK.
“Whilst there’s still a lot of work to do here, using knowledge of an individual’s biology to tailor the treatment plan should ultimately bring significant benefits to patients, both in survival and quality of life.”